Impact of Catheter Features on Clinical Outcomes
Access to the right intermittent catheter can be critical for clinical success; however, choosing
the right intermittent catheter is complex.4-7 Figure 1 reflects the number of considerations to make the right catheter choice. These include clinical condition, patient factors, and catheter features.4-7
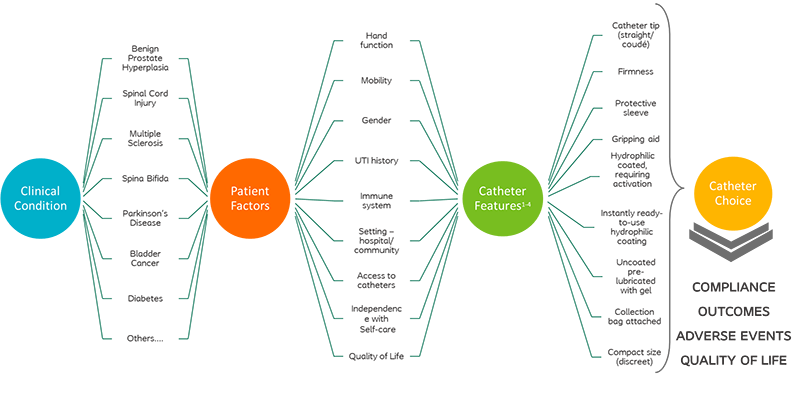
Figure 1. Complexity of Catheter Choice
Intermittent catheter
choice is individualized to meet the needs of the patient’s clinical condition.
For instance, patients with a spinal cord injury have various intermittent
catheter needs, related to the level and completeness
of injury, presence of spasticity, and need for a wheelchair. Therefore,
features that should be considered could be greater firmness, ready-to-use,
collection bag attached, packaging that is easy to open, a gripper and/or
protective sleeve, and hydrophilic coating or pre-lubrication. These features are related to the possibility of reduced or impaired hand function and mobility and an increase of infections. Table 1 lists patient needs for specific catheter features with the clinical rationale.
Table 1. Individualized patient needs correlate to specific catheter features supported by clinical rationale.
Clinical Condition |
Patient Needs |
Clinical Rationale |
Catheter Feature |
Spinal Cord Injury |
- Personalized based on level and completeness of injury
- Accessibility from wheelchair in multiple scenarios
- Difficult passing catheters due to spasticity
- Increased risk of infection, such as UTI/urosepsis
|
- Reduced/impaired hand function and mobility
- Increase risk of infections
|
- Greater firmness
- Ready-to-use (no activation)
- Attached to collection bag
- Easy to open packaging
- Gripper and/or protective sleeve
- Hydrophilic coating or pre-lubricated
|
Spina Bifida |
- Compliance with catheterization schedule as they transition into adulthood, including college/work/family life
|
- Minimizing adverse events and maintaining urethral integrity to support lifelong catheterization
|
- Discreet
- Hydrophilic coating or pre-lubricated
|
Multiple Sclerosis |
- Bladder management needs fluctuate with disease progression
- Prevent negative sequalae associated with poor bladder management
|
- Reduced or impaired mobility
- Impact neurological functions, including hand dexterity and body instability
|
- Discreet
- Ready-to-use (no activation)
- Protective sleeve
- Hydrophilic coating or pre-lubricated
|
Benign Prostatic Hyperplasia
|
- Accessibility through narrowed urethra and enlarged prostate
- Possible spastic sphincters
|
- Prostate enlargement narrows urethra
|
- Coudé tip with flexibility
- Protective sleeve
- Hydrophilic coating or pre-lubricated
|
Diabetes |
- Enhance compliance
- Reduce risk of infection, such as UTI/renal failure/urosepsis
|
- More ambulatory
- Increased risk of infections
- Multiple neuro comorbidities with advancing hand dexterity
|
- Discreet
- Introducer tips
- Hydrophilic coating
- Sterile kit (attached to collection bag)
|
Parkinson's |
- Decreased bladder control with disease progression
- Tangential loss of dexterity
- At risk of falls (most commonly in the bathrooms)
|
- Hand tremors and reduced dexterity
- Declining stability and mobility
|
- Greater firmness
- Ready-to-use (no activation)
- Attached to collection bag
- Easy to open packaging
- Hydrophilic coating or pre-lubricated
|
Bladder Cancer |
- Increased risk of infection, such as UTI/urosepsis
- Easy to catheterize in multiple situations
|
- Active chemotherapy reduces immune system
- More ambulatory
|
- Discreet
- Sterile closed kits
- Ready-to-use (no activation)
- Attached to collection bag
- Hydrophilic coating
|
Clinical complications associated with clean intermittent catheterization (CIC)
Long term users of CIC
are at a risk for potential complications. Factors such as improper hygiene,
incomplete bladder emptying, non-compliance with bladder management regimen,
inappropriate catheter choice, insufficient lubrication may contribute to increased
risk of complications.8 These complications could arise in the urethra
(such as bleeding, false passage) or the bladder itself (such as stones). A
comprehensive list of potential complications is outlined below. Despite
potential for these complications, CIC is the preferred method of bladder
emptying for long term bladder management.
Table 2. Complications Associated with Clean Intermittent Catheterization
Anatomical structure |
Complication |
Causes |
Urethra |
Urethral
bleeding or hematuria |
Tears or
injury of the urethra that are seen during the first months of intermittent
catheterization due to lack of technical expertise9; bleeding in
long-term patients may be a sign of other issues, including UTI |
|
Urethral
strictures |
Repeated
catheterization may result in inflammation and secondary, traumatic
strictures10 |
|
False passage |
Tract that is
created when a catheter is inserted through the urethral wall rather than the
lumen |
Scrotum or
testes |
Epididymitis
(Epididymorchitis) |
A rare inflammation
or infection of the epididymis of testes; common in men with urethral
strictures |
Bladder |
Bladder
stones |
Residual
urine is the primary cause of bladder stone; kidney stones entering the
bladder; introduction of pubic hair, or loss of the catheter, perforation,
residual urine, or necrosis of the bladder that surrounded by salt crystals
to create a stone11 |
|
Urinary tract
infections (UTIs) |
Bacteria
introduced into the urinary tract and bladder with catheter insertion;
urethral or bladder trauma from catheter; post-void residual urine from early
catheter removal or catheter inserted too far into the bladder3 |
Urethral Trauma
One
of the key outcomes, where hydrophilic catheters are speculated to make a
difference, is in relation to urethral trauma and microhematuria. The
hydrophilic technology adds a smooth wetted surface to the catheter and the
ability to impose lower friction force during catheterization, designed to reduce
risk of micro strictures and to protect the fragile mucosal lining of the
urethra.
One of the main
challenges in evaluating urethral microtrauma is the lack of standardization of
the outcomes, although the most common being hematuria. Indication of blood in
urine, urethral inflammatory response (such as leukocyte counts) are other
outcome measures. Even within the measured outcomes, varying methodology and
threshold levels across studies pose an ongoing challenge. Here, we present the
individual study data focused on friction force and hematuria.
Table 3. Literature associated with urethral trauma and associated hematuria.
Urinary Tract Infections (UTIs)
Urinary
tract infections (UTIs) are a risk for patients performing intermittent catheterization.3 Because the risk is lower with
the use of intermittent catheters than for indwelling catheters in neurogenic
lower urinary tract dysfunction, the American Urological Association (AUA) and
Society of Urodynamics Female Pelvic Medicine and Urological Reconstruction (SUFU)
guidelines recommend intermittent catheterization over indwelling catheters if
the patient is able to self-catheterize.16 On average, a CIC user will experience 0.75 to 2.7 UTIs/year, which
is significantly higher than the average population (internal Coloplast studies).
Three main reasons for the elevated UTI risk are the introduction of bacteria
into urethra, damaging of the epithelial cells (micro trauma) of the urethra,
weakening the defensive mechanisms and finally incomplete bladder emptying
leading to residual urine allowing growth of leftover bacteria which may cause
permanent bacteriuria (Figure 2).3 Long term sequalae
of UTI include frequent recurrences, pyelonephritis, urosepsis, renal failure
and high-level antibiotic resistance (due to prolonged antibiotic consumption, making UTI a major cause of morbidity in patients with NLUTD.17,18,19
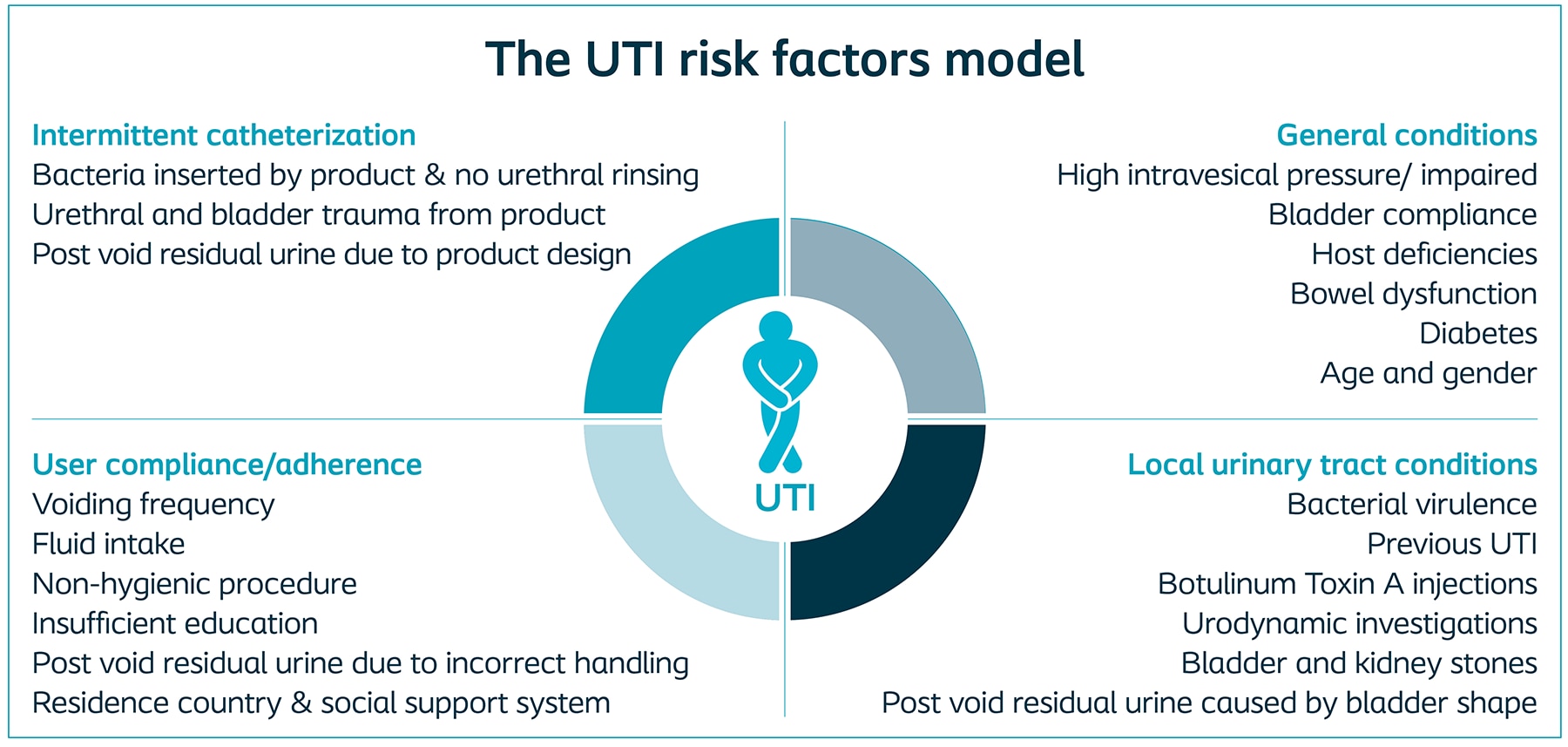
Figure 2. Graphic From: Kennelly M, Thiruchelvam N, Averbeck MA, Konstatinidis C, Chartier-Kastler E, Trøjgaard P, Vaabengaard R, Krassioukov A, Jakobsen BP. Adult Neurogenic Lower Urinary Tract Dysfunction and Intermittent Catheterisation in a Community Setting: Risk Factors Model for Urinary Tract Infections. Adv Urol. 2019 Apr 2;2019:2757862. doi: 10.1155/2019/2757862. PMID: 31065264; PMCID: PMC6466920.
Due to the known impact
of UTIs on the healthcare system, catheter features have been developed to
decrease the occurrence of this clinical complication. One of these features
includes hydrophilic coating. Notably, the importance of hydrophilic catheters
has been recently highlighted in the American Urological Association
guidelines.18
Here, we present the
individual randomized, controlled studies, which specifically look at the
impact of hydrophilic coated CIC on UTIs.
Table 4. Literature associated with urinary tract infections (UTIs)
Literature
cited
- Lapides J, Diokno AC, Silber SJ, Lowe BS. Clean, intermittent self-catheterization in the treatment of urinary tract disease. The Journal of urology. 1972;107(3):458-461.
- Wyndaele JJ. Complications of intermittent catheterization: their prevention and treatment. Spinal Cord. 2002;40(10):536-541.
- Kennelly M, Thiruchelvam N, Averbeck MA, et al. Adult Neurogenic Lower Urinary Tract Dysfunction and Intermittent Catheterisation in a Community Setting: Risk Factors Model for Urinary Tract Infections. Adv Urol. 2019;2019:2757862.
- Newman DK, New PW, Heriseanu R, et al. Intermittent catheterization with single- or multiple-reuse catheters: clinical study on safety and impact on quality of life. Int Urol Nephrol. 2020;52(8):1443-1451.
- Goetz LL, Droste L, Klausner AP, Newman DK. Catheters Used for Intermittent Catheterization. In: Clinical Application of Urologic Catheters, Devices and Products.2018:47-77.
- Newman DK, Willson MM. Review of intermittent catheterization and current best practices. Urologic nursing. 2011;31(1):12-28, 48; quiz 29.
- Newman DK. Teaching Tool: Methods and Types of Urinary Catheters Used for Indwelling or Intermittent Catheterization. Urologic Nursing. 2021;41(2).
- Herter R, Kazer MW. Best Practices in Urinary Catheter Care. Home Healthcare Now. 2010;28(6):342-349.
- Cardenas DD, Moore KN, Dannels-McClure A, et al. Intermittent catheterization with a hydrophilic-coated catheter delays urinary tract infections in acute spinal cord injury: a prospective, randomized, multicenter trial. PM R. 2011;3(5):408-417.
- Engberg S, Clapper J, McNichol L, Thompson D, Welch VW, Gray M. Current Evidence Related to Intermittent Catheterization: A Scoping Review. J Wound Ostomy Continence Nurs. 2020;47(2):140-165.
- Leslie SW, Sajjad H, Murphy PB. Bladder Stones. In: StatPearls. Treasure Island (FL): StatPearls Publishing. Copyright © 2021, StatPearls Publishing LLC.; 2021.
- Vapnek JM, Maynard FM, Kim J. A prospective randomized trial of the LoFric hydrophilic coated catheter versus conventional plastic catheter for clean intermittent catheterization. J Urol. 2003;169(3):994-998.
- Stensballe J, Looms D, Nielsen PN, Tvede M. Hydrophilic-coated catheters for intermittent catheterisation reduce urethral micro trauma: a prospective, randomised, participant-blinded, crossover study of three different types of catheters. Eur Urol. 2005;48(6):978-983.
- De Ridder DJ, Everaert K, Fernandez LG, et al. Intermittent catheterisation with hydrophilic-coated catheters (SpeediCath) reduces the risk of clinical urinary tract infection in spinal cord injured patients: a prospective randomised parallel comparative trial. Eur Urol. 2005;48(6):991-995.
- DeFoor W, Reddy P, Reed M, et al. Results of a prospective randomized control trial comparing hydrophilic to uncoated catheters in children with neurogenic bladder. J Pediatr Urol. 2017;13(4):373 e371-373 e375.
- Ginsberg DA, Boone TB, Cameron AP, et al. The AUA/SUFU Guideline on Adult Neurogenic Lower Urinary Tract Dysfunction: Treatment and Follow-up. J Urol. 2021;206(5):1106-1113.
- Biering-Sorensen F. Urinary tract infection in individuals with spinal cord lesion. Curr Opin Urol. 2002;12(1):45-49.
- B. Blok JP, D. Castro-Diaz,, G. del Popolo JG, R. Hamid, G. Karsenty, T.M. Kessler, Guidelines Associates: R. Boissier HE, B. Padilla Fernández TG, L. ‘t Hoen, S. Musco, V. Phé,, Schneider MP. EAU Guidelines on Neuro-urology. European Association of Urology. 2016.
- Flores-Mireles AL, Walker JN, Caparon M, Hultgren SJ. Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nat Rev Microbiol. 2015;13(5):269-284.
- Cardenas DD, Hoffman JM. Hydrophilic catheters versus noncoated catheters for reducing the incidence of urinary tract infections: a randomized controlled trial. Arch Phys Med Rehabil. 2009;90(10):1668-1671.
The materials and resources presented are intended to be an
educational resource and presented for general information
purposes only. They are not intended to constitute medical or
business advice or in any way replace the independent
medical judgment of a trained and licensed physician with
respect to any patient needs or circumstances. Please refer to
product ‘Instructions for Use’ for intended use and relevant
safety information. Considerations, techniques, practice, use,
and outcomes may vary based on clinical practice and
judgment.