icon
Intertrigo (or intertriginous dermatitis) is a rash that can develop in a skin fold. The condition is common and may affect people from infancy to adulthood. Certain factors increase your risk, such as having diabetes, being overweight, incontinence (unable to control bladder or bowels), wearing incontinence briefs, or being on bed rest.
Perspiration, warmth and friction may cause a skin fold to become red and inflamed. Symptoms such as itching, burning, odor and pain can accompany the redness. These symptoms can also occur under medical devices such as braces or splints, or adjacent to artificial limbs.
Common areas for intertrigo
Intertrigo may potentially develop in any skin fold or in areas where there is constant skin-on-skin friction (cf. 1). It may be found:
• Between thighs
• Under the armpit
• Under breasts
• Around belly folds
• Between fingers and toes
• In groin folds
• In neck creases
• Behind the knee
• Adjacent to an artificial limb
• Under a brace or splint
Other problems in skin folds
In someone who is incontinent, moisture from urine and stool can get trapped in skin creases. This may be found especially under the buttocks. The condition that develops is not intertrigo, but it is a type of dermatitis that can cause similar problems. When skin or a skin fold is moist and/or damaged, it is prone to infection from bacteria or fungus (cf. 1)
How to minimize the risk
For general prevention, patients should try to keep skin folds clean and dry, decreasing moisture and rubbing between folds of skin with a wicking fabric containing silver (cf. 2). InterDry® Ag Textile with Antimicrobial Silver Complex is a wicking textile that removes excess moisture, reduces friction and contains silver to help manage fungal or bacterial infections (cf. 3). It is also recommended that one wear lightweight, loose and absorbent clothing (cf. 4).
Caring for your skin
If intertrigo does develop, consider taking the following steps until the rash disappears:
Step 1: Wash the skin fold
- Wash gently, using a pH-balanced skin cleanser. Some options include a no-rinse body wash or no-rinse incontinence cleanser.
- Pat your skin dry. Do not rub.


Step 2: Protect your skin
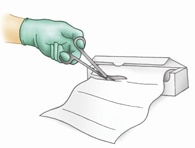
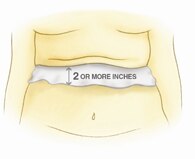
- Cut the appropriate size textile with scissors, allowing for a minimum of 2 inches of textile exposure outside the skin fold.
- Lay a single layer of textile into the base of the skin fold or under a medical
device such as a brace or splint. Leave at least 2 inches of the textile exposed outside the skin fold or brace/splint. This allows the excess
moisture to wick away from the skin fold and evaporate.
- Secure the textile in one of several ways: with the weight of the skin fold, with a small amount of tape or tucked into clothing.
- Remove the textile before bathing and replace it when finished.
- Replace the textile in 5 days or if it becomes soiled with urine or stool.
Patients should be sure to check their skin every day. They should look for rashes, redness, open areas; and inspect all skin folds, or under devices that rub against the skin.
Coloplast products for intertrigo
- Bedside-Care® Foam – pH-balanced, no-rinse cleanser
- InterDry® Ag Textile with Antimicrobial Silver Complex – The first effective solution for skin fold management. A wicking textile impregnated with silver to manage moisture, friction and fungal or bacterial infections3 in skin folds.